Guidelines
Due to continuous aging of population and increase in the number of elderly people, osteoporosis became socially significant disease leading to disability, increasing mortality and thereby putting an additional burden on the public healthcare system.
Screening to identify groups with a high probability of fracture is recommended using the FRAX® Tool for all postmenopausal women and men over 50 years old (А1). In the presense of major pathological fractures (hip, spine, multiple fractures) it is recommended to diagnose osteoporosis and prescribe treatment regardless of the results of spine and hip double X-ray absorptiometry (DXA) or FRAX® (B2).
It is recommended to evaluate C-terminal telopeptide when prescribing antiresorptive therapy and procollagen type 1 N-terminal propeptide (P1NP) when prescribing anabolic therapy to patients receiving osteoporosis treatment at baseline and 3 months after the start of therapy in order to assess the effectiveness of treatment early and adherence to the therapy (А2). It is recommended to diagnose osteoporosis and prescribe treatment to patients with high individual 10-year probability of major pathological fractures (FRAX®) regardless of the results of spine and hip DXA (В3).
It is recommended to diagnose osteoporosis and prescribe treatment with a decrease in BMD, measured by DXA, by 2.5 or more T-score standard deviations in femoral neck, and/or in total hip, and/or in lumbar vertebrae, in postmenopausal women and men over 50 years old (А2).
It is recommended to prescribe bisphosphonates, denosumab or teriparatide to prevent pathological fractures and increase BMD in patients with postmenopausal osteoporosis, osteoporosis in men, glucocorticoid-induced osteoporosis (А2). When the clinical effect of therapy in osteoporotic patients without pathological fractures is achieved (BMD T-score > -2.0 SD in femoral neck and absence of new fractures), it is recommended to interrupt bisphosphonates therapy for 1-2 years with subsequent follow-up (B2). In patients with vertebral fractures, hip fractures or multiple fractures, it is recommended to continue ceaseless long-term treatment of osteoporosis (В3).
All drugs for the treatment of osteoporosis are recommended to be prescribed in combination with calcium and cholecalciferol (А2). In order to reduce the risk of recurrent fractures by prescribing osteoporosis therapy timely and maintaining long-term follow-up of patients over 50 years old with pathological fractures, it is recommended to create Fracture Liaison Services (В2).
Original study
Background: Possible differences in the results of planned RCTs and real clinical practice were the reason for the analysis of long-term therapy with denosumab in patients with osteoporosis (OP) of various origins on an outpatient basis.
Aim: To assess the effectiveness of long-term administration of denosumab in terms of the effect on BMD and markers of bone metabolism, tolerance and consequences of drug withdrawal in patients with OP of various etiologies.
Materials And Methods: A retrospective analysis of the outpatient records of women with OP of various etiology, who were observed at the FSBI «NMRC TPM» from 1 to 10 years and regularly received denosumab 60 mg once every 6 months subcutaneously (at least 2 injections), was carried out. All completed examination and anthropometric research; DXA of the lumbar spine and proximal femur (PF); laboratory tests: marker of bone resorption CTx (β-crosslaps) in blood serum; survey on the presence of adverse events.
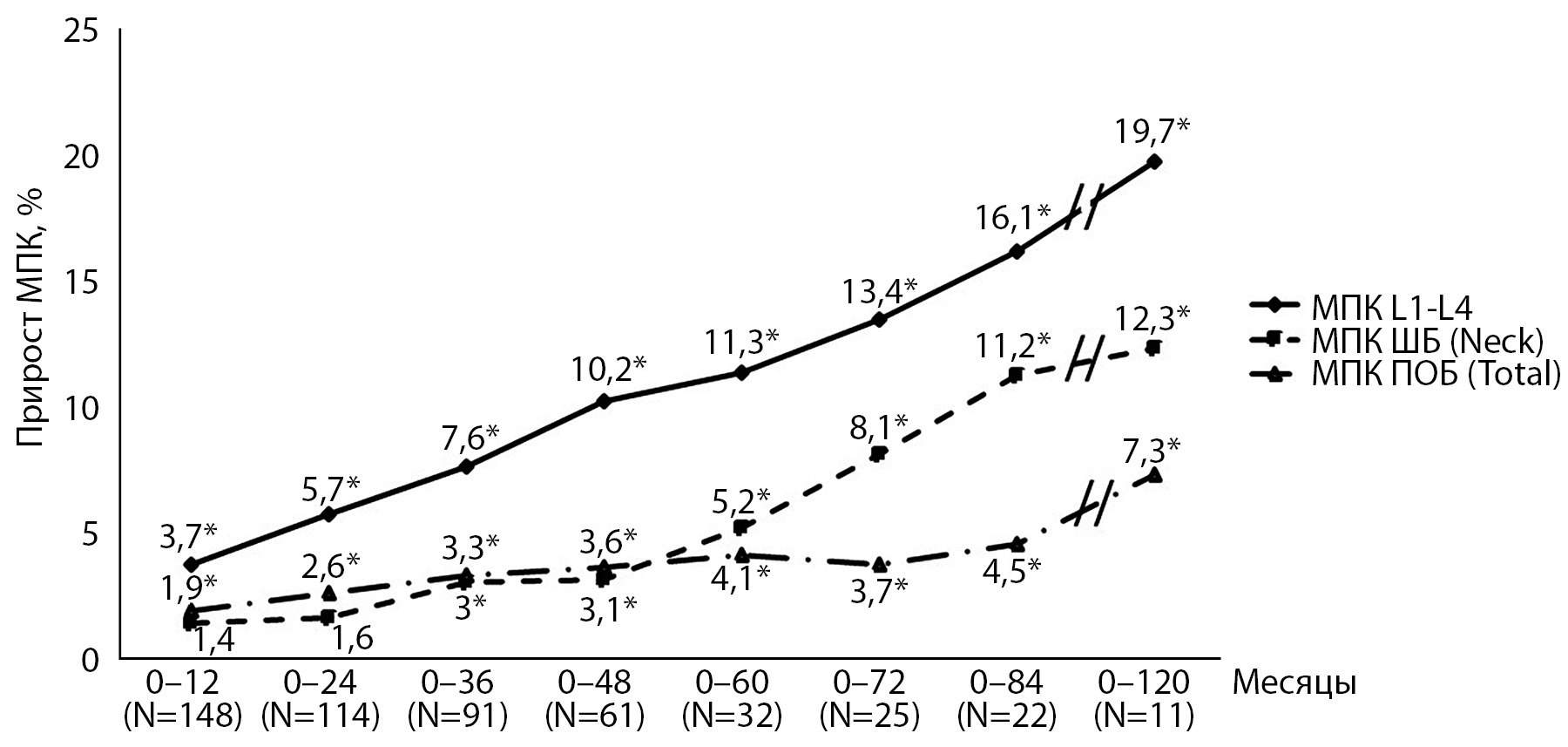
Results: The study included 148 patients who were divided into 2 groups: 1 (N=98) - did not take anti-osteoporotic therapy (AT), 2 (N=50) - who took AT before the appointment of denosumab. Long-term therapy with denosumab was associated with a steady and reliable increase in BMD in the spine and PF, as well as a decrease in the concentration of CTx of both those who didn’t take and who previously took AT. In 54% of patients BMD in the spine reached values of osteopenia, in 43.4% of women target BMD values in the femoral neck were determined. During the first year of therapy, there was a decrease in the concentration of CTx by 67% in those who didn’t take AT and by 58% in those who had previously taken AT. Discontinuation of denosumab therapy without subsequent administration of AT was associated with a significant decrease in BMD in the spine (by 4.4-8.2%) during the first year after discontinuation of the drug.
Conclusion: Denosumab therapy effectively increases BMD in the spine and PF and decreases CTx levels both in untreated patients and in those who previously received AT. It is necessary to discontinue therapy, further management of the patient should be discussed to prevent «withdrawal syndrome».
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2311-0716 (Online)