CLINICAL GUIDELINES
BACKGROUND: In Russia, according to official statistics, a high level of conservative treatment of fractures of the proximal femur remains, especially in older age groups. In this regard, assessing the effects of predictors of mortality at the stage of providing trauma care to such patients remains relevant. Тhere is ongoing debate regarding the timing of the effect of surgical treatment on mortality associated with the fracture event itself.
AIM: To assess the effect on mortality of hip fractures in people 50 years of age and older of the type of treatment (operative or conservative) and the duration of the preoperative period.
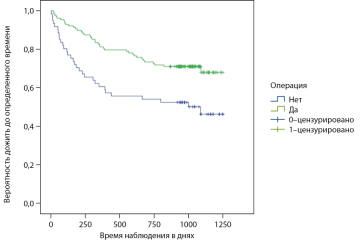
MATERIALS AND METHODS: A cross-sectional retrospective study with a prospective component was conducted on fractures of the proximal femur that occurred from January 1, 2019 to December 31, 2019 in people over 50 years of age living in the urban district of Armavir. The Kaplan-Meier method was used to analyze mortality.
RESULTS: Significantly longer survival after surgical treatment compared with conservative treatment was due to lower patient mortality in the interval up to 240 days (Breslow criterion (Generalized Wilcoxon, p<0.007) from the moment of injury Mortality by this period was, respectively, 11.7% versus 32.7%, the average mortality per day per 1000 patients is 0.489 among those operated on and 1.37 among those not operated on. In groups stratified by age and Charlson index, significant differences were noted only for persons 80 years of age and older. A delay in surgical intervention of more than 72 hours significantly increased mortality (Pearson chi-square test, log-rank test, p=0.012.
CONCLUSION: Surgical treatment performed within 72 hours of the hip fracture reduces or minimizes the risk of death associated directly with the fracture event itself, including in persons over 80 years of age. The effect of surgical intervention on mortality is maximally manifested in the time interval of 6-8 months after the fracture.
BACKGROUND: Vitamin D deficiency has shown a significant role in the impairment of muscle mass maintenance and skeletal muscle function, which are progressively reduced in sarcopenic patients with sarcopenia in the elderly. However, there are different points of view about the relationship between vitamin D deficiency and sarcopenia.
AIM: to assess the frequency and risk factors for vitamin D deficiency and identify the relationship with sarcopenia in people 65 years of age and older.
MATERIALS AND METHODS: the study included 230 people 65 years of age and older (median age 75 [68; 79] years) who completed a questionnaire using the Mini-Mental State Examination (MMSE), International Physical Activity Questionnaire (IPAQ). Sarcopenia was diagnosed according to EWGSOP2 criteria (2018). 25(OH)D was determined by enzyme immunoassay (Architect i2000SR, Abbot, USA).
RESULTS: there were no differences in age, gender, physical activity, smoking and other social characteristics between people with and without vitamin D deficiency (p>0.05). Vitamin D deficiency was detected more often in people with low BMI and obesity (p<0.001). Probable sarcopenia was detected in 64.8% of people 65 years of age and older, confirmed — in 28.7%, severe — in 21.3% of people. Vitamin D deficiency increased the risk of sarcopenia (OR=4.989; 95% CI 1.321–12.626; p=0.0420) and was associated with low muscle strength (OR=2.613; 95% CI 1.993–3.270; p=0.00116), low physical performance according to the results of the SPPB tests (OR = 1.905; 95% CI 1.342–2.710; p=0.00034) and the Timed Up and Go test (OR=1.364; 95% CI 1.003–1.853; p=0.047).
CONCLUSION: vitamin D deficiency was detected in 58.7% of elderly people and was associated with insufficient BMI and obesity. In sarcopenic patients, vitamin D deficiency was detected in 72.7% and was associated with age, BMI less than 25 kg/m2, low physical activity and low skeletal muscle function.
BACKGROUND: Different cytokines could affect bone tissue in patients with rheumatoid arthritis (RA). For formulation clinically significant conclusions about cytokines role in status of bone tissue in RA patients, actual studies are needed to obtain more data.
AIM: To study the association of bone mineral density (BMD) with immunological and humoral factors in postmenopausal RA women.
MATERIALS AND METHODS: The study included 73 postmenopausal women with RA (median age 63.0 [56.0; 67.0] years). A clinical and laboratory examination was performed including dual-energy X-ray absorptiometry to assess BMD of the lumbar spine (L1–L4), femoral neck (FN) and total hip (TH), level measurement of C-reactive protein (CRP), rheumatoid factor (RF), antibodies to cyclic citrullinated peptide (ACCP), parathyroid hormone (PTH), myostatin, follistatin, interleukin 6 (IL-6), IL-6 receptors, insulin-like growth factor 1, adiponectin, leptin, fibroblast growth factor 23, tumor necrosis factor (TNF) SF12.
RESULTS: Persons with osteoporosis (OP) have higher levels of adiponectin (p=0.002), TNF SF12 (p=0.015) and IL-6 receptors (p=0.014) compared to those without OP. L1–L4, FN and TH BMD positively correlated with leptin and IL-6; negative correlation was found between L1–L4 BMD and adiponectin, FN BMD and follistatin, TH BMD and TNF SF12 (p<0.05). Linear regression analysis revealed significant associations between L1–L4 BMD and PTH (β= -0.22), adiponectin (β=-0.36) and leptin (β=0.35); FN BMD with CRP (β=-0.23), ACCP (β=-0.21), PTH (β=-0.35), IL-6 (β=0.37) and leptin (β=0.32); TH BMD with CRP (β=-0.22), AСCP (β=-0.24), PTH (β=-0.30), adiponectin (β=-0.28) and leptin (β=0.42).
CONCLUSION: The conducted study showed that BMD in L1-L4, FN and TH is associated with the level of CRP, ACCP, PTH, adiponectin, leptin and IL-6 in postmenopausal women with RA.
REVIEW
Over the nearly 40-year history of dual-energy X-ray absorptiometry (DXA), the main focus has been on the diagnosis of low bone mineral density (BMD), i.e. osteoporosis, which has been the subject of many domestic and foreign publications. The problems associated with increased BMD and related not only to the difficulty of interpreting the results, but also to further patient management tactics have been covered significantly less. Most often, such cases pass unnoticed in routine clinical practice due to the orphan nature of many diseases leading to the development of pathologically high bone density, and, as a rule, are interpreted as a manifestation of osteoarthritis. Of course, arthrosis, scoliosis and other joint deformities (especially in the spine) are the cause of overestimation of BMD in most clinical situations. However, bone dysplasia, manifested by a diffuse or focal increase in BMD, can, like osteoporosis, be complicated by low-traumatic fractures; neurological and other complications, potentially leading to disability, also occur. Despite the extremely rare occurrence of these diseases, doctors’ insufficient awareness about the peculiarities of the clinical and radiological pattern and the course of sclerosing bone dysplasias can lead to errors in making a diagnosis, and first of all, to incorrect interpretation of the results of DXA. Our review aims to briefly describe genetically determined pathologies that cause an excessive increase in BMD, in order to attract the attention of the medical audience to this problem.
CASE REPORT
At the age of 3 years, the patient was diagnosed with chronic mucocutaneous candidiasis and at the age of 40 he developed autoimmune alopecia. At the age of 43, the patient began to complain of gradually progressive muscle weakness. At the age of 49, primary adrenal insufficiency and hypoparathyroidism were verified. Molecular genetic analysis revealed a mutation c.769C>T p.R257X in the AIRE gene, confirming the presence of autoimmune polyglandular syndrome type 1. Despite long-time stable compensation of adrenal insufficiency and hypoparathyroidism, the patient continued to experience progressive muscle weakness, leading to significant difficulties in walking and an inability to hold his head in an upright position. Based on the results of an extensive neurological examination and whole-genome sequencing, no hereditary myopathies were identified. Tests for myositis-specific antibodies were negative. An attempt to prescribe immunosuppressive treatment was unsuccessful.
Thus, we report progressive limb-girdle myopathy as one of the rare manifestations of APS-1, not associated with autoimmune damage to muscle tissue.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2311-0716 (Online)