CLINICAL GUIDELINES
Background. Fragility fractures (FF) determine main severity of medical and social consequences of osteoporosis. FF prophylaxis considers to prevent repeated fractures. For this reason special services are being created. Their principles and effectiveness require improvement and additional study.
Aim. Тo highlight key role of Fracture Liaison Services (FLS) for reducing incidence of FF by means of scientific publications and own material analysis.
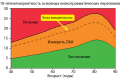
Materials and methods. Clinical material was collected at the Artashat Medical Center (Republic of Armenia). Study included 2,332 patients aged 50–97 years, including 1,656 women (71%) and 676 men (29%) with typical FF of limb bones. First group included 765 patients treated in 2011–2013, for whom anti-osteoporotic pharmacotherapy (AP) was prescribed due to known X-ray techniques. In second group of 1567 patients the AP was prescribed based on electronic FRAX calculator in 2014–2017. Proportions of patients in two clinical groups with and without AP were compares along with proportions who had repeated low-energy bone fractures. Moreover, past 20 years scientific publications analysis dedicated to prevention of FF and role of FLS was carried out.
Results. Comparative analysis revealed that patients proportion with prescribed AF based on use of FRAX calculator in second clinical group, significantly (p<0.05) increased by 16.6%, while patients proportion with repeated FF significantly (p<0.05) decreased by 6.5% (or 1.17 times) in relation to first group. Analysis of publications has shown high efficiency of FLS and their important role in reducing incidence of FF in general.
Conclusion. Use of FRAX calculator for AP prescription allowed to achieve significant (p<0.05) increase by 16.6% in proportion with prescribed specific AP, which led to significant (p<0.05) decrease of patient proportion (6.5%) with repeated low-energy fractures. Analysis of scientific publications and own material confirmed key role of FLS for reducing the incidence of FF.
REVIEWS
To reduce the frequency of fragility fractures, Fracture Liaison Services are being created worldwide. One of the most difficult parts in their organization is considered to be the creation of an effective system of long-term patient management. Many factors are involved in this process, concerning the patient, the team of specialist, the peculiarities of the organization of primary health care, and many others. On the one hand, it has been shown that the inclusion of patients in FLS increases their commitment to the implementation of doctor’s recommendations. On the other hand, there are a number of barriers depending both on the characteristics of the patient himself (polymorbidity, severity of the condition, decreased cognitive function, fear of side effects, low motivation to treat osteoporosis) and on various aspects in the medical care organization. The article analyzes the importance of training patients and medical personnel, approaches to the choice of therapeutic tactics, optimization of the process of succession management of patients, the availability of a system of information exchange between medical institutions. Using the example of the Yaroslavl’ FLS, the possibilities of improving various aspects of medical care are analyzed, as well as local problems that arose at various stages of the development of this service, and the measures that were applied to resolve them.
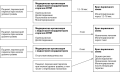
To prevent fractures which the elderly and the very old might deal with is a strategic task for preserving the life quality of the elderly and their independence from outside help, as well as reduce the health care and social support economic costs. The most effective and cost-effective organizational structure for reducing fractures frequency is the Fracture Liaison Service (FLS). The foundation of FLS at the regional level includes various models of these services, which is associated with a multi-level system of trauma care, different numbers of attached population and different number of specialists. Firstly, these are identification, assessment of clinical risk factors for osteoporosis, investigation for secondary osteoporosis causes and treatment initiation in the FLS with follow-up in the primary health care in 12–18 months’ time. Secondly, these are identification, risks assessment, patients’ investigation in the FLS during 3 months with the follow-up treatment initiating by the primary health care physician. And thirdly, these are assessment, investigation and treatment initiation by a primary care doctor immediately after trauma care. In any case of the FLS organization, a patient who has had a fragility fracture in any period after the fracture will be under the supervision of a primary care physician, and therefore additional efforts should be made by healthcare organizers, heads of a medical organization and other specialists in order to increase the identification of the patients with osteoporosis, their examination and treatment with anti-osteoporotic drugs in the primary health care. The article presents the results of the studies confirming the effectiveness of FLS with a coordinator, educational activities for patients and doctors, the role of a traumatologist in motivating a patient for examination and treatment, and other options to help a primary care physician with identifying, diagnosing and treating patients after fragility fractures.
In recent years Fracture Liaison Services (FLS) have been established worldwide to reduce the number of fractures due to osteoporosis. Within the framework of the global campaign «Capture the fracture» by International Osteoporosis Foundation (IOF), some questionnaires have been proposed to assess the quality of FLS’ organization. Key Performance Indicators (KPIs) are used to analyze the effectiveness of the FLS working at the patient level. Thanks to their use, it is possible to identify areas that need improvement, evaluate the effectiveness of the changes being made, and compare the quality of work in various FLS at the regional or country level. This article discusses approaches to the use and calculation of each KPI in practical healthcare in the Russian Federation, taking into account epidemiological data, national clinical guidelines, and the specifics of the organization of the healthcare system in our country.
CASE REPORT
Phosphaturic mesenchymal tumor can cause osteomalacia due to excessive secretion of fibroblast growth factor 23 (FGF23), which disrupts the metabolism of phosphate and vitamin D. These tumors are predominantly benign, but less than 5% of them are malignant forms. This article presents the first clinical case in the Russian Federation of a 69-year-old patient with severe hypophosphatemia due to metastatic prostate cancer. Increased secretion of FGF23 are described in the androgen-resistent prostate cancer, which led to pronounced disorders of mineral metabolism, accompanied by a clinical symptom of weakness, pain in the bones, immobilization of the patient. The condition was regarded as worsening against the background of the progression of the disease. However, symptomatic therapy aimed at increasing the level of phosphate significantly improved the patient’s general condition. The medical community should be aware of the possibility of developing hypophosphatemia in patients with weakness and bone pain, which are not always associated with the progression of metastatic prostate cancer.
SHORT REPORTS
The older people with osteoporosis, especially those with low-energy fractures, are the most vulnerable group of geriatric patients. They are shown the appointment of anti-osteoporotic therapy, which should be effective and safe. Unfortunately, the real prescription of medical treatment of osteoporosis in the world barely reaches 20%. This is due not only to low adherence to therapy by elderly patients, but also to financial and economic difficulties in obtaining drugs. For most patients, drug therapy for osteoporosis is quite expensive, especially given its long-term, often lifelong, course of action. However, new opportunities have now emerged to provide certain anti-osteoporotic drugs not only to patients in the preferential category, but also without disabilities. This will not only increase the number of patients receiving treatment for osteoporosis, but also reduce the risk of fractures, both primary and recurrent, the risk of falls, injuries and premature death among the elderly population.
The article presents modern possibilities of providing medicines to patients with osteoporosis and its complications in the form of pathological fractures using clinical and statistical groups (CSG) as new methods of payment for inpatient and hospital-replacing care in the Russian Federation.
ASBMR 2022 Annual Meeting and Vitamin D Workshop 2022 — the key international events in the field of metabolic diseases of the skeleton and pathology of mineral metabolism — were held in September 2022. During the conferences the results of the latest research were presented, promising areas of further research were discussed, as well as debates and author’s sessions on controversial issues were held. The article provides a brief overview of the events.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2311-0716 (Online)