Review
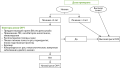
The analysis of contemporary publications devoted to the problem of medication-related osteonecrosis of the jaw (MRONJ) in patients receiving antiresorptive therapy is carried out. Since one of the most important risk factors for MRONJ is the dosage of the drug, this complication is much less common in patients with osteoporosis compared to cancer patients. The risk of MRONJ after tooth extraction when taking bisphosphonates for osteoporosis ranges from 0 to 0.15%, when taking denosumab — 1%. The basic rules for the management of a patient with osteoporosis receiving antiresorptive therapy in order to reduce the risk of developing MRONJ are formulated. These include consulting with a dentist before starting treatment for osteoporosis, especially in patients with high risk of MRONJ. It is necessary to maintain oral hygiene and perform invasive dental interventions before starting antiresorptive therapy. During the entire period of treatment of osteoporosis, it is necessary to pay attention to oral hygiene and timely conservative treatment of emerging problems. The patient should also be warned that when contacting the dentist, he should inform that he is receiving treatment for osteoporosis. A clinician engaged in the treatment of osteoporosis should know the signs of MRONJ and inform the patient about them. With the development of MRONJ, it is important to guide the patient with an informed dentist / maxillofacial surgeon. If an invasive dental intervention is necessary, the decision to discontinue treatment with bisphosphonates should be taken individually based on an analysis of the risk factors of the MRONJ and the severity of the intervention, and in the case of denosumab treatment, it should be carried out after 3–4 months after the last administration of denosumab. In some cases, it may be effective to add teriparatide to the combined therapy of MRONJ performed by a dentist / maxillofacial surgeon.
Original study
Background. Numerous studies have demonstrated the vitamin D role in the occurrence and development of various diseases. Despite the current treatment and prevention strategies, the problem of vitamin D deficiency prevalence among all the population segments remains unsolved.
Aim. To assess the prevalence of vitamin D deficiency and insufficiency among adult population living in the regions of the Russian Federation located at latitudes from 45° to 70°, as well as to analyze the life quality depending on the 25(OH)D serum level and determine the major associated risk factors for vitamin D deficiency.
Materials and methods. The Russian multicenter, non-interventional, cross-sectional registry study was conducted from October 2021 to March 2022 and included 499 participants.
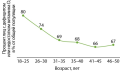
Results. According to the study, 69.14% of the participants had a vitamin D insufficiency or deficiency. The overall prevalence of vitamin D deficiency in autumn 2021 was higher than in autumn 2020. There were no significant differences in the prevalence of vitamin D deficiency among the Russian Federation regions. The 25(OH)D serum level depending on the sex of the participants was significantly different (p=0.002). Males had vitamin D deficiency in 43.72% of cases, and vitamin D insufficiency and deficiency in 75.7%. At the same time, the prevalence of vitamin D deficiency among the female was lower and amounted to 30.95%, while vitamin D insufficiency and deficiency — in the 62.7% of cases. In addition, vitamin D deficiency was most common in young adults in the age subgroup of 18–25 years (56.10%): the vitamin D insufficiency or deficiency was detected in 81.72% of participants by the statistical weighting methods. Generalized discriminant analysis showed that the biggest contributors to differences between presence and absence of vitamin D insufficiency or deficiency were the following: carbonated beverage consumption, weight, age, education, marital status, and dairy consumption.
Conclusion. Currently, there is a high prevalence of vitamin D deficiency in the Russian Federation, while there is no difference in the 25(OH)D serum level between the northern and southern regions. Male sex and young age (up to 25 years) are a high risk group for developing vitamin D insufficiency and deficiency. A wide range of vitamin D biological functions highlights the necessity of vitamin D insufficiency and deficiency treatment and prevention.
Background: The lack of accurate data on the prevalence of primary hyperparathyroidism (PHPT), the variety of clinical forms, the lack of routine biochemical screening of serum calcium levels, as well as the difficulty in the topical search for adenoma dictate the need for a detailed study of the clinical and laboratory features of PHPT.
Aim: Assess the clinical course and laboratory features of patients with PHPT in Tyumen region.
Materials and methods: A retrospective analysis of the case histories of 201 patients with PHPT who were hospitalized in the surgical department No. 2 at the Regional Clinical Hospital No. 1 in Tyumen in the period 2019–2021 was carried out. demographic and anthropometric data were studied, laboratory data (PTH, levels of total and ionized calcium, 25(OH)D) and instrumental (ultrasound) of the thyroid and parathyroid glands, CT and MRI of the neck organs with and without contrast were evaluated, scintigraphy of the parathyroid glands with technetrile) diagnostic methods.
Results: The incidence of PHPT in the Tyumen region was 5.8 cases per 100 thousand population in 2019, in 2020. — 3.2 cases in 2021 — 4.0 cases. The average age of all patients with PHPT was 60±11.05 years, 94.0% were women. The duration of the disease from the onset of the first symptoms to the time of diagnosis, on average, was 2.0±1.3 years. The manifest form of PHPT was detected in 80.1%, asymptomatic form in 17.9% of the examined, normocalcemic in 2.0% of patients. Among the main clinical manifestations of PHPT, the leading place is occupied by diseases of the cardiovascular system (n=157), manifested in the form of coronary heart disease, left ventricular hypertrophy, chronic heart failure in 68.1% of cases; in 86.9% arterial hypertension and cardiac arrhythmias in 6.9% of patients. Of the total number of patients, only 13.9% (n=28) had the level of 25(OH)D examined, of which 68% were diagnosed with a state of its deficiency or insufficiency.
Conclusion: Clinical manifestations of PHPT in the form of cardiovascular pathology dictate the need for a routine study of calcium levels in this category of patients, as well as clarification of the pathogenetic mechanisms underlying this relationship. The available data on the contribution of vitamin D deficiency to the development and progression of PHPT at the pre- and postoperative stage indicate need for study of 25(OH)D in this category of patients.
Background: Rheumatoid arthritis (RA) is an autoimmune inflammatory disease with a predominant joint lesion, as well as bones and muscles. The frequency of pathological phenotypes of body composition in patients with RA exceeds that in healthy individuals. Numerous factors can affect the body composition of RA patients, related to both the disease itself and lifestyle factors.
Aim: to assess the nutritional status and its relationship with phenotypes of body composition in women with rheumatoid arthritis.
Materials and methods: 91 women (average age 60.0 [51.0; 67.0] years) with RA underwent clinical and laboratory examination, dual-energy X-ray absorptiometry. Nutritional status was assessed using the Mini Nutritional Assessment (MNA) questionnaire.
Results: in total, the risk of malnutrition and malnutrition was identified in 44% of the examined patients. Correlations were established between the nutritional status by MNA and total and appendicular muscle mass (r=0.30, p=0.003 and r=0.35, p=0.001, respectively), between body mass index and bone mineral density (BMD) of lumbar spine (r=0.23, p=0.030), BMD of femoral neck (r=0.30, p=0.004) and the BMD of total hip (r=0.33, p=0.001). Multivariate analysis revealed the association of sarcopenic phenotype with nutritional status by MNA <24 points (OR 2.85 (95%CI 1.05–7.69), p=0.039), daily calcium intake <500 mg/day (OR 2.74 (95%CI 1.01–7.45), p=0.048) and upper arm circumference <25 cm (ОR 6.02 (95%CI 1.48–24.53), p=0.013). The obesity phenotype was associated with the risk of malnutrition (ОR 4.97 (95%CI 1.33–18.54), p=0.018) and upper arm circumference >25 cm (ОR 4.07 (95%CI 1.21–13.77), p=0.024). The phenotype of osteoporosis was associated with age >55 years (ОR 7.81 (95%CI 2.12–28.80), p=0.002), nutritional status by MNA <24 points (ОR 1.45 (95%CI 1.06–1.96), p=0.019) and sarcopenic phenotype (ОR 4.57 (95% CI 1.38–15.13), p=0.013).
Conclusion: the frequency of low nutritional status was 44% among the examined women with RA. It was revealed that all pathological phenotypes of body composition were associated with a reduced nutritional status according to MNA.
Case report
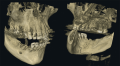
The article is a description of a clinical case of osteonecrosis of the mandible in a patient receiving antiresorptive therapy on the background of breast and thyroid cancer (diagnosis was established in 2011). A year later, courses of chemotherapeutic treatment were started, zoledronic acid 4 mg was administered parenterally, and then Denosumab 120 mg. 9 years after the start of chemotherapy in the clinic at the place of residence, the patient’s teeth 4.4 and 4.5 were removed, within two months there were no signs of healing of the bone wound, in connection with which the dentist-surgeon performed an audit of the sockets of the extracted teeth, which provoked a deterioration in the condition of the tissues of oral cavity, decreased quality of life of the patient. Four months after the extraction of teeth 4.4 and 4.5 the patient turned to the dental clinic of the Tver State Medical University, where she is stil lreceiving complex antibacterial, anti-inflammatory and restorative treatment. The patient’s well-being and quality of life have been improved.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2311-0716 (Online)