CONSENSUS
Bisphosphonates are the most commonly used drugs for the treatment of osteoporosis and reducing the risk of fractures, which were introduced into clinical practice more than 30 years ago. The bisphosphonate group includes oral (alendronic acid, risedronic acid, ibandronic acid) and parenteral (zoledronic acid, ibandronic acid) preparations. By now, quite large groups of patients with osteoporosis have been taking bisphosphonates for a long time. This fact raises questions about the preservation of the clinical effect, the development of side effects of drugs against the background of prolonged administration, as well as the possibility of cessation or interruption in their use. The document contains recommendations of the experts of the Russian Association for Osteoporosis on the management of patients with osteoporosis receiving bisphosphonate therapy based on the literature review and discussion. The recommended duration of treatment with oral and parenteral bisphosphonates, methods for monitoring the effectiveness of treatment, as well as signs that should be used when deciding on a discontinuation of the therapy or an increase in its duration are formulated. The criteria of ineffectiveness of treatment requiring its correction are discussed. A separate section is devoted to monitoring the patient during a ‘drug holiday’ in taking bisphosphonates and making a decision on resuming treatment. Recommendations are also given for the control and prevention of possible side effects and increasing persistence to bisphosphonate treatment.
We present a consensus on high dose cholecalciferol (Devilam 5000 IU and 50000IU) prescription in clinical settings. There was a expert committee meeting to reach a consensus on the recommendations for endorcrinologists, primary care physicians and primary care specialists to prevent and treat vitamin D deficiency in various groups of patients. The expert committee reached a consensus on prescribing prophylactic doses of vitamin D in daily, weekly and monthly regimes to prevent vitamin D deficiency without vitamin D measurements. A single dose of cholecalciferol 50 000 IU should be prescribed to patients with low traumatic fractures and/or requiring antiresorptive treatment for osteoporosis when vitamin D measurement is not available. Treatment doses (50 000 IU per week) of vitamin D should be reserved for patients with established vitamin D deficiency (< 30ng/ml). Considering the prevalence of vitamin D deficiency in Russia, the expert committee suggested that all people require prophylactic doses of vitamin D from November to April, whereas the elderly (65+) benefit from whole year vitamin D supplementation. There is a group of people with vitamin D metabolism abnormalities associated with hypercalcemia (genetic or granulomatosis disorders) who should avoid vitamin D. On the other hand, patients with obesity, malabsorption and osteomalacia require higher doses of vitamin D for longer periods of time. High-dose vitamin D formulation in matrix form (50,000 IU, 5,000 IU) is a high-dose vitamin D preparation within the framework of the registered instructions for the prevention (in intermittent dosing mostly) and treatment of vitamin D deficiency/insufficiency. Taking into account the rapid achievement of a therapeutic effect, good tolerability, safety of the drug and the convenience of intermittent administration to achieve greater patient compliance with the treatment, the expert committee has come to the conclusion that high-dose vitamin D formulation in matrix form should be recommended in different group of people to be given according to this consensus.
CLINICAL GUIDELINES
BACKGROUND: The lack of sufficient systematization of data on the use of bisphosphonates for primary prevention of osteoporotic fractures in postmenopausal women with osteopenia prompted us to conduct a systematic review with meta-analysis of publications devoted to this problem.
AIM: To study the effect of bisphosphonates on bone mineral density (BMD), markers of bone metabolism and fractures in postmenopausal women with osteopenia.
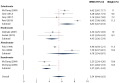
MATERIALS AND METHODS: A total of 1140 potentially eligible articles were found in the initial publication screening. From the initially identified results, 13 studies were meta-analyzed. The design of the studies selected for meta-analysis was consistent with randomized controlled trials.
RESULTS: On average, study bisphosphonate preparations compared with placebo increased lumbar spine BMD by 5.54 % (95 % CI 4.44–6.63, I2 = 93.65 %), total hip BMD by 4.53 % (95 % CI 3. 2–5.86, I2=96.32 %), femoral neck BMD by 3.63 % (95 % CI 1.5–5.75, I2=95.9 %), total body BMD by 3.25 % (95 % CI 2.28–4.22, I2=87.87 %), proximal femur BMD by 4.76 % (95 % CI 3.43–6.08, I2 = 88.64 %). There was a statistically significant effect of bisphosphonates on low-energy fractures (OR 0.62; 95 % CI 0.49–0.77), clinical vertebral fractures (OR 0.51; 95 % CI 0.38–0.69), and radiologically confirmed vertebral fractures (OR 0.63; 95 % CI 0.4–0.98).
CONCLUSION: These results obtained allow us to conclude that bisphosphonates (alendronate, zolendronic acid, ibandronate, resedronate) have a positive therapeutic effect, and their administration is justified in postmenopausal women with osteopenia for the prevention of osteoporotic fractures and increase in BMD.
BACKGROUND: Vitamin D deficiency in secondary hyperparathyroidism (SHPT) against the background of chronic kidney disease (CKD) in patients with diabetes mellitus (DM) is one of the key factors in the deterioration of renal function.
AIM. To assess the indicators of calcium-phosphorus metabolism in individuals with SHPT against the background of CKD, diabetes and without it to optimize treatment approaches.
MATERIALS AND METHODS. A retrospective analysis of 416 medical records with diagnoses CKD3-C5 and SHPT was carried out, of which 112 had a history of diabetes, which were examined and treated in the nephrology department of the in the period from 01. 01. 2018 to 31. 12. 2022. Demographic and anthropometric data were studied, laboratory (total and ionized calcium, total protein, albumin, phosphorus, creatinine, parathyroid hormone, 25(OH)D, alkaline phosphatase) and instrumental (ECHO-CG, ultrasound of the abdominal organs and retroperitoneal space) research methods.
RESULTS. Diabetes is the leading cause of CKD among all nosological forms. The level of 25(OH)D in patients without diabetes varied from 9.04 to 152 nmol/l, with diabetes from 8.3 to 77 nmol/l. The average level of 25(OH)D in patients without diabetes (41.7 ± 26.1 nmol/l) was significantly higher than in patients with type 1 diabetes (20.3 ± 14.9 nmol/l) and type 2 diabetes (27.6 ± 19.2 nmol/l) (p = 0.005 and p = 0.003, respectively). 25(OH)D deficiency and insufficiency were more often recorded in patients with diabetes compared with patients without carbohydrate disorders (89 % and 10 % versus 69 % and 19 % respectively), while the optimal level was more common in patients without diabetes (12 % and 1 %, respectively).
BACKGROUND: Microarchitecture of trabecular bone tissue can currently be evaluated using a special program for dual-energy X-ray absorptiometry (DXA) to determine the trabecular bone score (TBS).
AIM: to assess bone microarchitecture and fracture risk in patients with rheumatoid arthritis (RA).
MATERIALS AND METHODS: a cross — sectional study included 95 postmenopausal women with confirmed diagnosis of RA (mean age 62.3 ± 8.1 years). The survey was conducted using a specially designed questionnaire, laboratory examination, DXA of the lumbar spine (L1–L4) with the determined of TBS and proximal femur. The risk of major osteoporotic fractures (MOF) was assessed using FRAX calculator without or with TBS standardization.
RESULTS: 41 (43.2 %) patients had osteoporosis (OP) in at least one measurement area, while in L1–L4 — 26.3 %, in the femoral neck (FN) — 22.1 % and in total hip (TH) — 11.6 % persons. 35.8 % women had normal, 25.3 % — partially degraded and 38.9 % — degraded microarchitecture according to TBS. In patients with a history of fractures, low TBS was detected significantly more often than in people without fractures (p < 0.05). TBS was negatively correlated with age with age (r = -0.30, p = 0.003), duration of postmenopause (r = -0.26, p = 0.014), cumulative dose of glucocorticoids (GCs) (r = -0.34, p = 0.045) and positively correlated with BMD L1-L4 (r = 0.43, p < 0.001), BMD of the FN (r = 0.21, p = 0.038) and BMD TH (r = 0.23, p = 0.02). Normal BMD values in L1–L4 and at the same time degraded microarchitecture according to TBS were in 9.5 % RA persons. A high risk of fractures according to FRAX was detected in 47 (49.5 %) women, and FRAX adjusted for TBS increased the number of such patients to 52 (54.7 %).
CONCLUSION: OP was diagnosed in 43.2 % of postmenopausal women with confirmed RA, and 38.9 % had degraded bone microarchitecture by TBS. Negative associations were found between TBS and age, duration of postmenopause, cumulative dose of GCs, and positive associations with BMD in all parts of the skeleton. Including TBS values into the FRAX calculator made it possible to redistribute patients into risk groups, as a result of which 54.7 % of patients had a high risk of MOF.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2311-0716 (Online)